Parents’ and Caregivers’ Health Insurance Supports Children’s Healthy Development
Edited by Rebekah Levine Coley, Ph.D., Boston College. For more information, contact Kelly R. Fisher, Ph.D., Director for Policy, Society for Research in Child Development, at policy@srcd.org.
Author
- Elisabeth Wright Burak, M.P.P., M.S.W., Center for Children and Families, Georgetown University
When adults’ health care needs are met, they are better equipped to support their children as they grow and learn. When just one uninsured family member faces high medical costs or untreated conditions, the resulting stress can harm children’s well-being throughout their lives. Lack of health insurance is associated with limited access to needed care, poorer health outcomes, and financial instability,1 all of which can inhibit children’s healthy development. Since 2013, millions of Americans have gained health insurance under the Affordable Care Act (ACA) through Medicaid or new marketplaces. Children living in states that expanded Medicaid to adults are more likely to have health insurance themselves. But after years of progress, recent reversal of health insurance growth threatens children’s health and development.
Health Coverage Gains Have Stagnated
Medicaid, the Children’s Health Insurance Plan (CHIP), and the ACA have dramatically improved access to affordable health insurance coverage among children and parents, but progress has stalled. Increased Medicaid eligibility for children over more than two decades, accelerated by creation of CHIP in 1997, has reduced the rate of uninsured children to record lows—less than 5 percent in 2016.2 The ACA, fully implemented in 2014, helped millions of adults—including many parents—gain affordable health insurance for the first time, leading to dramatic declines in the number and percentage of uninsured Americans under age 65.
- Despite progress, health insurance gains among parents stalled in 2017 (see figure), with nearly 7 million parents3 uninsured.4,5 Parents with children 3 and younger are uninsured at even higher rates (20.4 percent in 2016).
- In 2017, the rate of uninsured children increased for the first time in nearly a decade to 5 percent (4 million). In just one year, 276,000 children joined the ranks of the uninsured.6
- Health insurance rates vary by state. Parents and children living in states that adopted the ACA Medicaid expansion are far more likely to be insured than those in non-expansion states,7 and this gap is growing.8
Uninsurance Rates Among U.S. Parents Ages 19-64
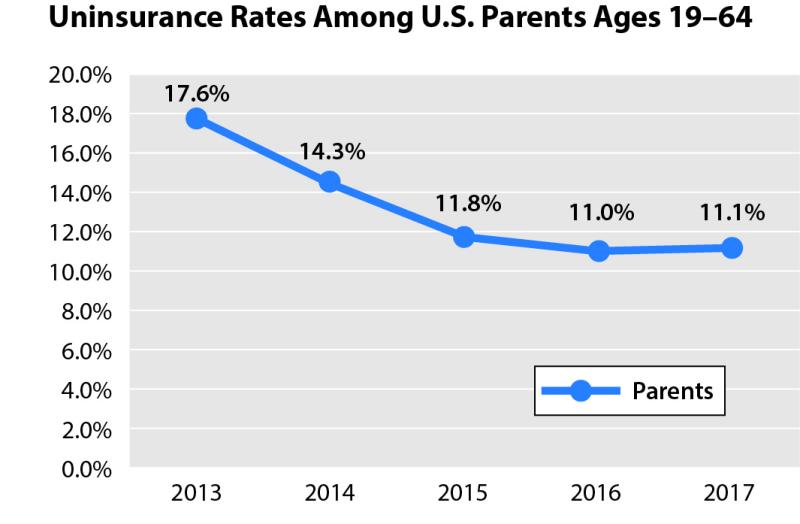
Source: Urban Institute analysis of 2013–17 American Community Survey data from the Integrated Public Use Microdata Series. Estimates reflect an adjustment for potential misreporting of coverage on the American Community Survey. As published in Haley, J., Kenney, G.M., Wang, R., Pan, C., Lynch, V., & Buettgens, M. (2019). Improvements in Uninsurance and Medicaid/CHIP Participation among Children and Parents Stalled in 2017. Urban Institute. Retrieved from https://www.urban.org/research/publication/improvements-uninsurance-and-medicaidchip-participation-among-children-and-parents-stalled-2017.
Parents Are Central to Children’s Development
Interactions with parents and caregivers shape children’s brain structure, cognitive and emotional development, and long-term ability to thrive.9 But poor health or lack of access to care can impair parents’ ability to support children’s development. Researchers estimate that when a parent reports their own health as good or excellent, their child is more than three times as likely to be in good health than a child with similar demographic and household characteristics and parents in fair or poor health.10 Untreated conditions, such as depression, impede parents’ capacity to bond with and care for their children, inhibiting healthy development.11
In contrast, insurance coverage improves parents’ and children’s well-being. Studies show that adults who gained insurance coverage through the ACA’s Medicaid expansion had greater access to treatment and improved health outcomes.12 For example, ACA Medicaid expansion is strongly associated with declines in both maternal13 and infant14 mortality rates. Being uninsured also affects otheradults who contribute to children’s development, like grandparents, child care providers, and teachers.
Health Insurance Improves Families’ Financial Security
Poverty and financial strain can harm a child’s wellbeing— from birth weight and nutrition to brain development and educational success.15,16 For many families, medical bills are a major source of financial strain. One study estimated that more than 60 percent of all bankruptcies in 2007 were due to medical costs.17 A growing body of research shows that health insurance— especially through Medicaid—improves families’ economic security18 by limiting out-of-pocket health care costs.19 The rate of families reporting problems paying medical bills has decreased since 2011,20 as has the amount of non-medical debt sent to third-party collection agencies.21 Parents living in states that expanded Medicaid under the ACA report decreased psychological stress, likely associated with reduced financial burden.22
When Parents Gain Health Insurance, So Do Their Children
Children’s access to public health insurance is linked to better health, education, and career outcomes in adulthood.23 Years of research show that providing health insurance for parents also improves coverage for children who are not already enrolled in Medicaid or CHIP.24 After the ACA, this so-called “welcome mat” effect was largest among children whose parents gained insurance through Medicaid.25 Research also shows that when parents gain health insurance, their children are more likely to receive regular preventive check-ups.26
Improving Children’s Outcomes
Providing health insurance for parents and caregivers is an important two-generation strategy to boost children’s long-term outcomes. Evidence suggests that improving parents’ and caregivers’ access to health insurance will also improve the health and well-being of the next generation. Increased access to health insurance also improves access to services, decreases financial strain, and provides peace of mind that parents and children can get the health care they need when they need it.
Endnotes / References
(1) Kaiser Family Foundation. (2018). Key facts about the uninsured population. San Francisco, CA: Author. Retrieved from https://www.kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population/
(2) Alker, J., & Pham, O. (2018). Nation’s progress on children’s health coverage reverses course. Washington, DC: Georgetown University Center for Children and Families. Retrieved from https://ccf.georgetown.edu/wp-content/uploads/2018/11/UninsuredKids2018_Final_asof1128743pm.pdf
(3) In this context, parents are defined as adults ages 19 to 64 living with their children ages 18 or younger.
(4) Haley, J., Kenney, G.M., Wang, R., Pan, C., Lynch, V., & Buettgens, M. (2019). Improvements in uninsurance and Medicaid/CHIP participation among children and parents stalled in 2017. Washington, DC: Urban Institute. Retrieved from https://www.urban.org/research/publication/improvements-uninsurance-and-medicaidchip-participation-among-children-and-parents-stalled-2017
(5) Haley, J., Wang, R., Buettgens, M., and Kenney, G. (2018). Health insurance coverage among children ages 3 and younger and their parents in 2016. Washington, DC: Urban Institute. Retrieved from https://www.urban.org/sites/default/files/publication/96141/medicaid_chip_2001686_0.pdf
(6) Op. cit. (2)
(7) Haley, J., Kenney, G.M., Wang, R., Pan, C., Lynch, V., & Buettgens, M. (2018). Medicaid/CHIP participation rates rose among children and parents: Variation in 2016 and recent trends. Washington, DC: Urban Institute. Retrieved from https://www.urban.org/sites/default/files/publication/99058/uninsurance_and_medicaidchip_participation_among_children_and_parents_updated_1.pdf
(8) Op. cit. (4)
(9) Center on the Developing Child at Harvard University. (2016). From best practices to breakthrough impacts: A science-based approach to building a more promising future for young children and families. Cambridge, MA: Author. Retrieved from https://developingchild.harvard.edu/resources/from-best-practices-to-breakthrough-impacts/
(10) Murphy, D., Cook, E., Beckwith, S., & Belford, J. (2018). The health of parents and their children: A two-generation inquiry. Bethesda, MD: Child Trends. Retrieved from https://www.childtrends.org/wp-content/uploads/2018/10/AECFTwoGenerationHealth_ChildTrends_October2018.pdf
(11) Murray, L., & Cooper, P.J. (1997). Effects of postnatal depression on infant development. Archives of Disease in Childhood, 77, 99-101. Retrieved from https://adc.bmj.com/content/77/2/99
(12) Antonisse, L., Garfield, R., Rudowitz, R., & Artiga, S. (2018). The effects of Medicaid expansion under the ACA: Updated findings from a literature review. San Francisco, CA: Henry J. Kaiser Family Foundation. Retrieved from https://www.kff.org/report-section/the-effects-of-medicaid-expansion-under-the-aca-updated-findings-from-a-literature-review-march-2018-appendix/#Nation1
(13) Rosenberg, J. (2019). Medicaid expansion linked to lower mortality rates. American Journal of Managed Care. No vol., n.p. Retrieved from https://www.ajmc.com/conferences/academyhealth-2019/medicaid-expansion-linked-to-lower-maternal-mortality-rates
(14) Bhatt, C., & Beck-Sagué, C. (2018). Medicaid expansion and infant mortality in the United States. American Journal of Public Health, 108, 565-567. Retrieved from https://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.2017.304218
(15) American Academy of Pediatrics (2016). Poverty and child health in the United States: Council on community pediatrics. Pediatrics, 137, n.p. Retrieved from https://pediatrics.aappublications.org/content/137/4/e20160339
(16) Evans, G.W., & Cassells, R.C. (2013). Childhood poverty, cumulative risk exposure, and mental health in emerging adults. Clinical Psychological Science, 2, 287-296; Santiago, C.D., Wadsworth, M., & Stump, J. (2011). Socioeconomic status, neighborhood disadvantage, and poverty-related stress: Prospective effects on psychological syndromes among diverse low-income families. Journal of Economic Psychology, 32, 218-230; Cohen, S., Janicki-Deverts, D., Chen, E., & Matthews, K.A. (2010). Childhood socioeconomic status and adult health. Annals of the New York Academy of Sciences, 1186, 37-55.
(17) Himmelstein, D.U., Thorne, D., Warren, E., & Woolhandler, S. (2009). Medical bankruptcy in the United States, 2007: Results of a national study. The American Journal of Medicine, 122, 741-746. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/19501347
(18) Also see Op. cit. (12)
(19) Sommers, B.D., & Oellerich, D. (2018). The poverty-reducing effect of Medicaid. Journal of Health Economics, 32, 816-832. Retrieved from https://www.sciencedirect.com/science/article/pii/S016762961300091X?via%3Dihub; Remler, D.K., Korenman, S.D., & Hyson, R.T. (2017). Estimating the effects of health insurance and other social programs on poverty under the affordable care act. Health Affairs, 36, 1828-1837. Retrieved from https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2017.0331
(20) Cohen, R.A., & Zammitti, E.P. (2018). Problems paying medical bills among persons under age 65: Early release of estimates from the National Health Interview Survey, 2011-June 2017. Hyattsville, MD: National Center for Health Statistics. Retrieved from
https://www.cdc.gov/nchs/data/nhis/earlyrelease/probs_paying_medical_bills_jan_2011_jun_2017.pdf
(21) Hu, L., Kaestner, R., Mazumder, B., Miller, S., & Wong, A. (2018). The effect of the patient protection and Affordable Care Act Medicaid expansions on financial well-being. Cambridge, MA: National Bureau of Economic Research. Retrieved from https://www.nber.org/papers/w22170
(22) McMorrow, S., Gates, J.A., Long, S.K., & Kenney, G. M. (2017). Medicaid expansion increased coverage, improved affordability, and reduced psychological distress for low-income parents. Health Affairs, 36, n.p. Retrieved from https://www.healthaffairs.org/doi/10.1377/hlthaff.2016.1650
(23) Wagnerman, K., et al. (2017). Medicaid is a smart investment in children. Washington, DC: Georgetown University Center for Children and Families. Retrieved from https://ccf.georgetown.edu/wp-content/uploads/2017/03/MedicaidSmartInvestment.pdf
(24) Op. cit. (7)
(25) Hudson, J.L., & Moriya, A.S. (2017). Medicaid expansion for adults had measurable ‘welcome mat’ effects on their children. Health Affairs, 36, n.p. Retrieved from https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0347; also see Committee on the Consequences of Uninsurance, Institute of Medicine. (2002). Health insurance is a family matter. Washington, DC: National Academy Press; Center on Budget and Policy Priorities. (2006). Coverage of parents helps children, too. Washington, DC: Author. Retrieved from https://www.cbpp.org/research/coverage-of-parents-helps-children-too
(26) Venkataramani, M., Pollack, C.E., and Roberts, E.T. (2017). Spillover effects of adult Medicaid expansions on children’s use of preventive services. Pediatrics, 140, n.p. Retrieved from https://pediatrics.aappublications.org/content/140/6/e20170953